This week's writer has a five year old girl. A few different situations and feelings are explained, which I think many parents of children with PDA will relate to. We have definitely been there ourselves with the sleep issues, and the overriding anxiety.
I am a 46 year old mother of three children. Two boys aged 15 and 13 from my first marriage and one little girl aged five with my second husband. My eldest son A has a diagnosis of ASD. When he was nearly 1, he had his first seizure and after 4 more, he was eventually treated for epilepsy for two years. Meanwhile, my youngest son M by the age of three months was very poorly, his hair was falling out, he lost a lot of weight, he was in pain after every bottle and his eyes were permanently red and finally after being repeatedly told he had colic, he was diagnosed with an allergy to cows’ milk protein. He then began to thrive. My first husband and I got divorced when both boys were under three.
When A started nursery the teachers alerted me to the fact that they believed he was autistic…he would repeatedly do jigsaw puzzles and play alongside his peers, but rarely with them. Then began a four year journey to diagnosis, as A could be sociable, could make eye contact and could present himself well (hold it together) in public but at home, he had regular violent meltdowns for a host of different reasons and a change in routine would send him into a spin. CAMHS eventually diagnosed him once we were allowed to see them (our paediatrician repeatedly said A wasn’t autistic and blamed my parenting skills suggesting I was ‘tearful’).
My youngest son M (20 months younger than A) is neurotypical in every way and was brought up in the same way….he had to have a period of counselling which I sought out for him after years of verbal abuse/put downs from his brother which crushed his self-esteem. They are very close as teenagers and A’s autism is barely apparent at present; meltdowns are now triggered only by his sister’s screaming or heightened embarrassment at which point he will now ‘roar’, invariably throw something and regrettably now (which I gather is quite common), swear in the most inappropriate way he can seem to think of in front of his five year old sister. He is then deeply ashamed afterwards but can’t say sorry (just the way he is).
This brings me to the current situation with our daughter, W. Since starting the primary school nursery at age three, W displayed signs of separation anxiety and screamed every day that I left her almost every day of the two years that she attended nursery. She was happy at nursery and calmed soon after I left. When she started school we expected a fairly fluid transition as everything was familiar to her. We expected her to be upset when I left each day but it escalated to her anxiety being so great that she ‘couldn’t’ eat – she wanted to eat and felt hungry but couldn’t get the food down as her tummy ‘felt sick’ all the time. She barely ate for two weeks and because she has been diagnosed with Cyclical Vomiting Syndrome after 4 overnight hospital stays on a drip, we ended up back in hospital for blood tests. W has a terrific fear of needles, blood and hospitals after a bad first experience with a failed drip so this was challenging but they got the blood and the results were clear. The hospital said it could only be a psychological problem and suspected anxiety.
The primary school were amazing and a plan was devised whereby I would go in to school each day with W for an hour; she would have her lesson, be guided by the picture exchange cards the school had out for her so she knew what to expect, and then W and I would leave together after a calm hour. We did this for some time to build confidence and trust and after half term she felt able to let me work in the staff room while she managed a whole school day independently (she occasionally came to me for reassurance but that soon passed and I was able to return to work away from school).
Since then, W has come on in leaps and bounds with school and has actively enjoyed saying goodbye on the days she could do it without tears. Even on the days with tears, she soon settled with her teacher and at the end of the school day was happy to report how ‘great’ her school day had been. We still had some issues with meltdowns after school and very definite sensory problems e.g. repeatedly having to put on each item of clothing until it felt ‘right’ – often resulting in big tantrums when they didn’t (even though we painstakingly tried to ensure the clothes were unlikely to cause issues). Then the virus struck.
Initially, W coped very well as she is already practised in washing her hands because of her vomiting condition. She enjoyed us all being together and was engaged in her set work from school and celebrated her achievements. Over the last few weeks however, we have seen a big change in W. She has never been a great sleeper but since her difficulties last September, she has been unable to settle herself to sleep without me in the bedroom with her (albeit with me reading and refusing to engage once story-time is over). This has now changed to her getting hysterical if I don't lie next to her and I'm not even 'allowed' to read a book for the two hours I'm there as she feels I'm not looking after her well enough if she doesn't have 100% of my attention and even moves my arms/legs to where she thinks they should be. She used to still be asleep by around 8pm though.
Now it’s almost as though W has forgotten how to sleep and gets very distressed about bedtime no matter how comforting the usual ritual, how many sleep aids we use (we’ve tried everything from music, audio books, lighting, sound boxes, meditation, weighted blankets, cuddle toys, pillow spray, warm baths, warm milk etc, but nothing works and she now actively rejects all sleep aids). She thrashes about saying she can’t sleep and gets very distressed very quickly and says she just feels scared when I’m not in direct contact with her (which I’m trying to avoid as much as possible at bedtime after the initial night night cuddle).
It’s getting later and later every night no matter what I try. I tried (with W very much on board) the 10 minute sleep routine where I go up after every 10 minutes with little communication until she is supposed to fall asleep. She was so pleased with herself and managed 7 rounds of 10 minutes after which time she was so stressed about lying there waiting for me to return despite being pleased with herself that she’d done it (?!), she had gone way past sleep and was then a shaking screaming ball of distressed fury screaming “I can’t stop crying, I can’t calm down, what’s wrong with me?”. It took me until 11.20pm that night to get her settled and only then by me lying holding her tightly. Controlled crying is not an option – because she can’t calm herself down once upset and also because of the knock-on effect of her brother’s reaction at the screaming. Her Daddy, as much as she loves him, is not an adequate replacement for me it would seem – everything has to be me.
This sleeping issue is what has lead me to desperation. In my experience over the last however many years, I have learnt that no behaviour exists without a ‘reward’ – to behave a certain way, you must be gaining something from it. In W’s case, her ‘obsession’ with me and having me nearby I believe comes from anxiety certainly but also from some extreme insecurity – she can only gain the security she needs from my physical presence it seems. My question that I can’t answer alone is why? She is loved, has a very secure home, she isn’t short of attention or care. She was traumatised from a young age by her older brother’s loud meltdowns and used to physically shake so it possibly started there but we have compensated for that so much at this point, I’m baffled as to why she should feel that way.
Her words are that she “misses my kindness” when I’m not near her (even downstairs or the next room is too far away for her). W also had the cow’s milk protein allergy as a baby together with silent reflux (which she was medicated for) so she was in pain a lot as a young baby and had to be carried more as it was the only way to relieve her discomfort. The strong attachment to me was probably formed as early on as that. This was all written before I had the PDA lightbulb moment and I now know that in the case of PDA, there is no 'reward' from the behaviour, it exists out of uncontrollable anxiety.
W hears everything and sees everything – she picks up on the finest detail no matter how cryptic or disguised our conversations have had to become, especially since the onset of coronavirus (the word sends her into a spin and she can no longer watch TV programmes for fear of it being mentioned in an advert). I am in a situation now where she seeks my attention for most of the day (I’m trying to work from home since lockdown which is now very challenging because of this). I have no evening because I am upstairs with her trying to settle her until on average 9.30/10pm every night and it’s having an impact on the rest of the family as I can’t spread myself any thinner!
I spent almost a whole day revisiting old basic tools I used with our son when he was younger and from yesterday began to use a host of picture exchange cards at home for W along with the ‘now’ ‘next’ system to break it down for her. These seemed to work quite well and we had a better day as she took comfort from them. I will reserve judgement as it’s early days yet. We have devised a new tick chart as well for her to use each time she goes to the toilet and washes her hands independently as she has been getting extremely distressed about that lately and her sensory problems seem to be resulting in her losing the feeling of being ‘empty’ in her bladder so she thinks she constantly needs to go (she doesn’t have cystitis). She then doesn’t want to go to the toilet alone, hates the feeling of wee on her skin and has started to hate washing her hands even though she knows she has to and is terrified of Covid-19 and so it goes on! The tick chart is helping a little bit. None of this worked but I have left it in to demonstrate I have tried a number of different strategies.
I have also ordered a blackout tent for her to retreat to with stress balls, light up sensory toys etc when she feels overwhelmed. This is becoming quite challenging behaviour and I’m keen to manage it as best I can. The sleep issue I’m not succeeding in and it is now taking its toll on W and on all of us as a family. We need help.
To summarise, this is what we’re currently seeing in our daughter:
Challenging / controlling behaviour, mostly directed at Mum
Sensory issues : distressed by loud noises; repeating phrases or tunes repeatedly; compulsively sniffing things (she used to have to lick them too which has halted for now); clothing sensitivity; very picky eater and won’t try anything preferring instead the same very limited foods; she likes playing with water but if she gets wet unexpectedly she struggles to deal with it no matter how hard we try to ‘fix it’/dry her.
Toileting issues much worse – she feels she keeps needing a wee but says she doesn’t want to go but then feels she has to go so then ensues the issue of washing her hands which she doesn’t want to do but knows she must. She often doesn’t feel that she’s got all the wee off her skin so toilet times have generally become quite distressing. She NEVER wants to go to the toilet alone and will try any tactics to get us to go with her / wipe her / wash her hands with her. We are trying a reward chart for this with mixed results.
She is often extremely irritable but like Jekyll and Hyde with it. She goes from being really wild to suddenly acting like an angel and back to her loving caring self like nothing has happened.
Extreme phobia of blood, needles, hospitals, doctors – anyone having a ‘baddie’ especially herself – if she falls over, it’s mayhem.
Almost obsessive attachment to her teddy who she says came to life for a moment the other day and ever since she has started dressing him in a nappy and clothes and insisting that she can’t go to bed until he has pyjamas on, nappy off, teeth brushed in a particular way etc.
She struggles to entertain herself and has become quite focused on hide and seek games and wants to play the same game repeatedly
If she receives my constant attention she stays on a more acceptable level but this isn’t sustainable to the level she would want it.
Hyper-sensitive even when playing – if things don’t go her way, she is liable to ‘flip out’ unexpectedly with a loud angry outburst. She might wake in a really happy loving mood and then for no apparent reason just switch into a terrible, irritable angry awkward mood that nobody can seem to help her with – it usually goes as fast as it arrived.
She says she wants to be a baby and will sometimes try to get into one of her dolls nappies and only speak with “goo goo ga ga” words. She recently saw a photo of herself as a baby and said she didn’t ever want to see it again because it made her sad and wished she was still like that.
She is self-deprecating despite constant reassurance that she is good at a lot of things and kind, caring, funny etc. She gets annoyed with herself that she ‘can’t do things’ and she says she’s stupid and wishes she wasn’t like ‘this’. She seems to be very aware of her tantrums and unreasonable behaviour afterwards and gets distressed even though we tell her we understand.
There have been several incidents at school where W has not coped. For example, she watched an episode of Go Jetters on CBeebies which featured a cartoon story of the fatbergs in London sewers and for hours afterwards, we couldn’t get her to go to the toilet because she was convinced that the toilet would flood and poo would go everywhere. She held on to her wee and poo for so long that she then really struggled to go – we had to show her how a toilet works, show her that that was a cartoon exaggeration of the fatbergs and real ones aren’t that big, explain that could never physically happen etc. It took about three hours and more work again for a few days afterwards to get her to settle and even now she is terrified of CBeebies and YouTube in case Go Jetters comes on unexpectedly. Similarly, she is afraid of nearly every Disney film, and nearly everything on children’s TV has made her ‘scared’ at some point so now she can only watch BabyTV.
She is afraid of a lot of things (blood, spiders, unexpected noise etc) and shakes with distress / goes red in the face / cries a lot so doesn’t seem to be doing it for attention – the fear can often be something really unusual and benign but it’s real to her and we struggle to calm her despite good tactics and reasonable logic.
She struggles when ‘on task’ to leave something incomplete even though often it seems ‘complete’ to us.
When excited / focused / concentrating, her arms and facial expressions become rigid, sort of pursing her lips with apparent delight (my son used to pull the same face and flap).
This isn’t an exhaustive list, I’m just recalling the more obvious things to give whoever might read this a reasonable overview.
In summary, we are coping with the day to day and I have given an overview of my personal background to hopefully demonstrate that I’m not entirely new to this. I have raised and steered a now 15 year old autistic boy away from violent, self-harming unacceptable behaviour to a boy who is liked by his mainstream teachers and peers and who has managed to develop his own coping strategies to get through life happily, now managing his own time constraints and demands of school (he tells me he’s not autistic and I’ve made it up!). What we aren’t coping with is the sleep deprivation and the apparent trauma that the inability to self-soothe and get herself to sleep (even with help) seems to be causing W and the family unit.
Thanks for taking the time to read. Comments are much appreciated and sharing on social media could really help get these posts to people who have still not heard about PDA.
For more reading about what Pathological Demand Avoidance is, please see 'Challenging Behaviour and PDA', and for an idea of how to help please read Strategies For PDA.
There's a chance PDA can be misdiagnosed as ODD (Oppositional Defiant Disorder) but there is a distinct difference. More information can be found here: the difference between PDA and ODD.
A variety of experiences of living with PDA can be read using the link Our PDA story series.
If you feel up to sharing your own experiences with my readers to help spread understanding (this can be anonymously), please email stephstwogirls@gmail.com.
The PDA Society website has a huge range of information about Pathological Demand Avoidance.
To find out more about our experiences, please check out our 'About Us' page. If you are looking for more information on Pathological Demand Avoidance, the posts below may help.
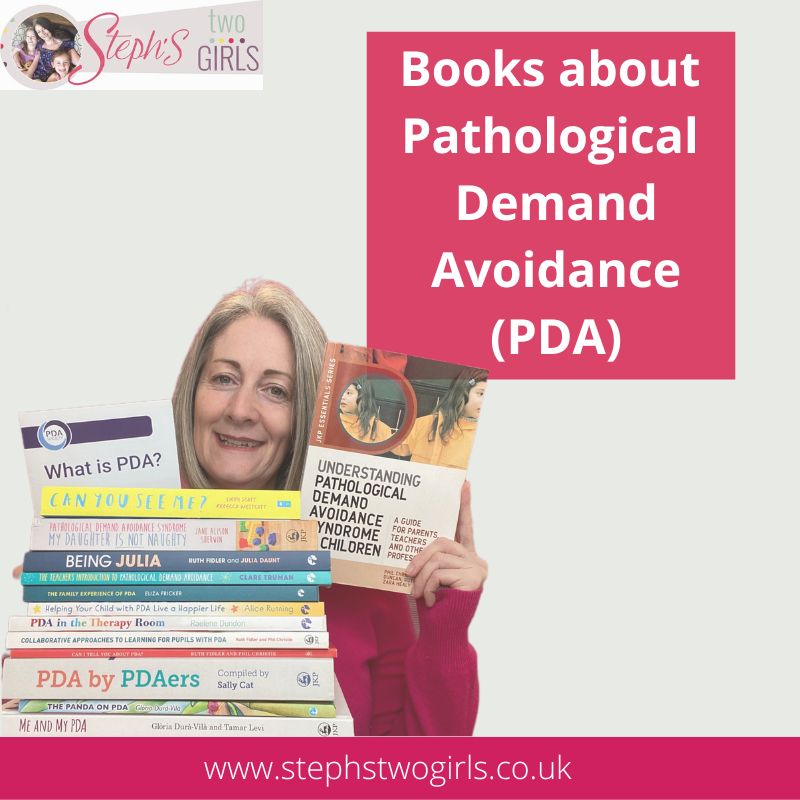
Books about the Pathological Demand Avoidance (PDA) profile of autism
What is PDA (Pathological Demand Avoidance)?
Ten things you need to know about Pathological Demand Avoidance
Does my child have Pathological Demand Avoidance?
The difference between PDA and ODD
Strategies for PDA (Pathological Demand Avoidance)
Pathological Demand Avoidance: Strategies for Schools
Challenging Behaviour and PDA
Is Pathological Demand Avoidance real?
Autism with demand avoidance or Pathological Demand Avoidance?
To follow me on other social media channels, you can find me at the following links or click the icons below!



















Hello 46 years young mother, It sounds like an exhousting job to keep the daily life going for you. So first of all a big compliment for the job you have done so far!
ReplyDeleteI think the struggle between not giving your children (especially your youngest) too much of everything the way they want it versus making them feel comfortable and avoiding anxiaty must be challenging. At least that is how I feel with my children.
I work with autistic children and I am a mother of 3 Doughters. The problems we have at home are less extreme, but I do recognise a lot. My girls are not diagnosed, but I know they have their problems that would fit into the spectrum. And I would sertainly call my husbant PDA, we live in Germany and here PDA is not a given diagnosis (yet).
Maybe I can help you with ideas/strategies that I found helpfull...
The first thing I thought was: 'Why practice being without momy and falling asleep all in one.' I think it could be helpfull to splitt these 2 things and start the 'trying to be alone for a few minutes without distraction' during the day, without the expactation of her to fall asleep.
I find it helpfull to tell my kids that it is ok if they can not sleep and tell them what I will think about (Things we did together during the day) while they are in their beds, then we mosly desite to think about the same (happy) moments and then I can leave the room.
Also I have had to explain to my oldest that it is OK for her to come to me if anything is wrong. She said: 'Really, but you said I have to stay in bed?' so maybe clearing that might also make your girl feel more in controll.
You wrote that she gets enough attention, but in her opinion she doesn't... It might seem the most impossible thing in the stressfull daily life you discribe, but maybe it could help to spent more 1 on 1 time with her, where the daily stress gets forgotten and she feels seen (follow her ideas of what to do in this time). Even if only 5 minutes in the evening, my children are so much more compliant and peacefull after I do this.
At the time my middle one (6 yrs) shows a lot of avoidance and objection. I finaly found my way to handle this, so that I do not have to avoid any conflict anymore: It helps a lot to confront her with a phisicall 'fight' where she gets a chance to let her strength out against me, without hurting me. She pushes me over and I push her down and cuddle her. This gives her a way back to being happy together with me, without losing the fight about the initial point (for example wearing socks in winter). She knows where the border is and sometimes experiments how far she can go, by kicking or boxing me, but there I just stop the game and tell her clearly that that is never ever allowed. It also gives me a good feeling that there is something I can do to help her, because on her own she would really struggle a lot with her own resistance against demands. And I can tell my other 2 kids to stay away from her whenn she feels like this, because I will take care of it (because her reaction to comforting would be inpredictable and sometimes physically agressive and both her sisters do want to comfort her whenn she is struggeling alone)
OK, that was a lot of information about my situation, maybe it will help you somehow...
By the way, have you tried Melatonin or any stronger medication? I am not a fan of medication, but I think in some cases it could just give the entire familiy the break they need to get the strength to cope wihth the problems. Also melatonin I would really call completely harmless.
Are there any organisation in your country that help people in your situation by, just doing things with the children, so that you could have some time for yourselve?
I wish you and your familiy all the best!