Pathological is a word that wasn't in my everyday vocabulary, until I had a 'lightbulb moment' upon hearing the phrase Pathological Demand Avoidance many years ago. Our younger daughter had been diagnosed with autism but she seemed in many ways different to other autistic children (certainly those whose parents I met with at that time). Standard suggested approaches for helping autistic children didn't seem to work with her, and everyone seemed to be at a loss as to why. Then I stumbled across the PDA Contact group (which in 2016 registered as a charity, the PDA Society) and realised that the characteristics of PDA that were being described fitted our daughter to a T.
PDA also explained how she was finding it impossible to control her extreme reactions to everyday demands. This was not toddler tantrum behaviour; it was distinctly different to how our older daughter reacted to society's expectations and everyday life. Initially, our younger daughter's verbal communication and understanding seemed slightly delayed, and her reactions to simple requests would feel extreme. For us, this didn't translate as violent meltdowns but more as withdrawal (more often than not into a 'mushroom position') and avoidance. As she grew older her speech and language improved and instead of outright refusing she would come up with varied and sometimes wild reasons for not being able to do as we requested, such as 'I can't do that because my legs don't work'.
PDA has been described as an anxiety-driven need for control. That seemed to fit our daughter, although the anxiety wasn't generally so obvious when she was younger. Control of situations was what she seemed to need, but she never realised that she was controlling. Her understanding of the world was slightly behind her peers at that time so it wasn't control in a calculated way. Nowadays her extreme anxiety about many things is clear to see - travel, being anywhere new, social situations, sensory issues, weather conditions and more - but that could be described as a more typically autistic characteristic. The need for control, or maybe autonomy is a better word, was, and is, different to that 'typical' kind of anxiety.
What's in a name?
Pathological wasn't a word I had used much before our lightbulb moment. The definition, according to the Oxford Learners dictionary, is:
- not reasonable or sensible; impossible to control
- caused by, or connected with, disease or illness
There are negative connotations associated with it; many people would probably link the word pathological with 'liar'. As in, someone who can't stop telling lies. Initially I cringed at the thought of this connection and felt slightly uncomfortable using that term. In the following years I blogged regularly about our life with PDA in the family, and I stopped thinking about the meaning of the word pathological, possibly because I began to use the acronym PDA instead. Quicker to say, and write, and avoids using the awkward word.
The origins of the name Pathological Demand Avoidance are not disputed; it was first coined by Elizabeth Newson in the 1980s. Professor Newson was a well respected developmental psychologist who was awarded the OBE for services to children on the autistic spectrum in 1999. She observed a number of children in her clinics and over the course of a few years, she identified a group who had similar characteristics to each other but who did not fit the standard criteria for autism at that time. They were all given the diagnosis of atypical autism, a term that came under the banner of Pervasive Developmental Disorder. However, Professor Newson felt that this term didn't do a good job of describing how these children were different from other autistic children, so she chose the name pathological demand avoidance syndrome in order to be more descriptive and group them together. She believed that knowing about the pathological degree of demand avoidance would help doctors, psychologists, and teachers to consider the child's characteristics more, and blame the parents or child less.
Discussions about whether this profile of autism should be called something else seem to pop up every so often online. Some have suggested that PDA could have been better named as a Pervasive Demand Avoidance or Persistent Drive for Autonomy. Others thought Extreme Demand Avoidance would have been a preferable choice. The latest phrase that seems to have come into play is 'a persistent and marked resistance to demands'.
The National Autistic Society has recently changed the information on its page about PDA. I have been wavering about whether to mention this because I thought drawing any attention to it would not be helpful. However it couldn't be ignored forever and I am aware of the growing feelings of frustration at how a national charity could be so invalidating to a large part of its own community. I definitely won't link to the new page, because I think it's confusing and misleading. I would go as far as to say it could be harmful, for parents who are starting their 'journey' in the same way we were 14 years ago. There seem to be conflicting views shared and it feels as though the NAS has been pressured into backtracking from their previous stance and several successful conferences they held on the subject of PDA.
There are a few other labels that are sometimes suggested instead of PDA - worth considering for some, but not an explanation for our girl.
Challenging Behaviour
Or, as Dr Ross Greene would call it, behaviour that challenges us. Our daughter's behaviour challenged us to think differently, to parent differently, in a way we hadn't needed to for our older daughter. Our PDAer wasn't violent, or aggressive; when refusing she would use social strategies and language rather than just say no, and when entering a state of meltdown there would be a lot of crying and hysterics but she would curl up into a mushroom shape or hide under a duvet.
Many children with PDA don’t display any aggressive behaviour, but some PDAers become so anxious (in a world which often doesn’t understand them, and which they often struggle to understand) that they become physically aggressive towards other people or the environment, perhaps as a way of trying to take back some control, often subconsciously. The important thing to remember with PDA is that this behaviour is anxiety based, so in effect a panic attack. Very often when the child is provided with a lower demand, more appropriate environment, the aggression and anti-social behaviour lessens, because the child feels less overwhelmed and out of control.
Oppositional Defiant Disorder (ODD)
This article from the National Library of Medicine* is well worth a read. It states that according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the main feature of ODD is a persistent pattern of angry or irritable mood, argumentative or defiant behavior, or vindictiveness toward others. In the DSM-5, the criteria for an ODD diagnosis are:
- Often loses temper
- Often touchy or easily annoyed
- Often angry and resentful
- Often argue with authority figures or, for children and adolescents, with adults
- Often actively refuse or defy to comply with requests from authority figures or with rules
- Often deliberately annoys others
- Often blames others for his or her mistakes or misbehavior
- The child has been spiteful or vindictive at least twice within the past 6 months
On the Good Schools Guide website, one relatable quote from a parent states:
‘I think for me the difference I found was that when I was told he was ODD I got tougher with him… but it still wasn't helping, and was in fact exacerbating the problems. It was only after getting the PDA diagnosis that I began to notice whilst he was refusing to do things it was more so in relation to something that was causing anxiety, for example going into shops, school etc. Then I began to also notice that he was displaying the behaviours to avoid demands.’
Conduct Disorder (CD)
This article, again from the National Library of Medicine**, shares that Conduct Disorder is a pattern of behaviors that demonstrate aggression and violation of the rights of others and evolves over time. These include:
- Aggression to people and animals: bullying, threatening, initiating fights, using weapons, physically cruel to people and animals
- Destruction of property: deliberately causing damage to property, setting fire
- Deceitfulness and theft: often lies, breaks into other’s house, car, shoplifting, forgery
- Serious violation of rules: stays out late at night, frequent running away from home, school truancy.
None of these have ever applied to our child. For any child who they do apply to, I would think the bigger picture needs to be considered and specialist help involved.
Attachment Disorder
Dr Judy Eaton is a Consultant Clinical Psychologist and Clinical Director of the Help For Psychology clinic. According to her blog post Autism, PDA or Attachment, the proposed criteria for Developmental Trauma Disorder are that "there must be evidence of exposure to ‘multiple or prolonged adverse events over a period of at least one year’. This means repeated and severe domestic violence; significant disruption of caregiving, repeated changes of caregiver, or exposure to severe and persistent emotional abuse."
Trauma
Trauma is a word that is sometimes brought up as a reason for demand avoidance or for not being able to comply with demands. Trauma can cause a wide range of physical and emotional symptoms (although it's important to note that not everyone who experiences a stressful event will develop trauma). In the early years, before our daughter was diagnosed, and in the first few years that followed, there was no trauma in our family or to her more specifically.
The only way in which the word trauma could be attributed to her life at all is some years down this path, after some of her school experiences. She went on to create an animation about this (that I'll share here because I'm proud of her self-taught skills and the effort she put into this!) but this has in no way influenced any of our thoughts about PDA as this didn't happen until several years after her early diagnosis.
ADHD crossover
ADHD is a diagnosis that is commonly found alongside autism, and I would guess that many PDA children might also have ADHD. Some of the outward behaviour signs may be similar. But not all PDA children can be explained, instead of using the term PDA, as having autism with ADHD. PDA demand avoidance is different. Our younger daughter is not diagnosed with ADHD. Our older daughter is, however, and for that reason I know that ADHD doesn't necessarily always show up obviously in outward behaviour.
ADHD was suggested for our younger daughter when she was around 6 years old, but the results from the initial Conners ratings scale questionnaire for ADHD we were given at that time were divided - school didn't think she showed enough of the criteria, whereas what we as parents had ticked about her behaviour at home would have indicated she did have ADHD. The decision was made to not follow through and offer a full assessment - the overall opinion was that it was her PDA behaviours that were more dominant anyhow. And as her demand avoidance has always prevented her from taking any medicine (see my post Top tips when your child won't take medicine!), there was no chance of ADHD medication helping her! But the point is, her presentation cannot be described as autism and ADHD, the demand avoidance is more than that.
I'm not a medical expert of course, but I am an expert in my own children. I could try to tell you everything that has happened to us over the last 16 years but it would take a long time (some of that will be in our soon-to-be-published book, PDA in the Family!). I can clearly see the difference between our two girls, and can tell you why I believe one can be described as having PDA and one not. It's a challenge to capture it all in just a few words in a blog post, and even my book doesn't have enough words to explain it all... maybe I should write a thesis on it?!
I understand that every individual is different and there can be many factors that affect families in different ways, from social environments to responses from within families, and the different levels of support received (or not). So I can't speak for every family, and I'm not trying to. I've been telling our story over the years to help other families not feel so alone, and to help them figure out what might help their children. I think there are many more people who know about PDA now compared to fourteen years ago when I first heard the term. Some of those will feel that this term is a good fit for their child too. Are they right? I don't know, I'm not an expert in those children. But I think most families wouldn't choose to use this term unless they needed to. I believe it is far easier to parent in a typical, traditional manner - that's what we did with our eldest daughter, and it worked fine. There was no need to suggest PDA described her.
For us, finding the term PDA led us to information that we needed to be able to understand our younger daughter better. It helped us learn how to support her. If we had only been able to use the term 'autism', I am sure fewer people would have understood why she acted the way she did. Pathological Demand Avoidance is a more accurate descriptor for her. I hope that vital research can be undertaken to understand more about individuals who present with these characteristics.
What matters most in all of this is of course not what term is used for PDA, but what understanding there is of how the demand avoidance can be all-encompassing for these children, and how different approaches are more successful than those typically suggested for autism. Several years ago I wrote a post titled Strategies for PDA, summarising what worked for us at home, and I highly recommend checking out all the valuable information on the PDA Society website: What helps? Guides.
Resources
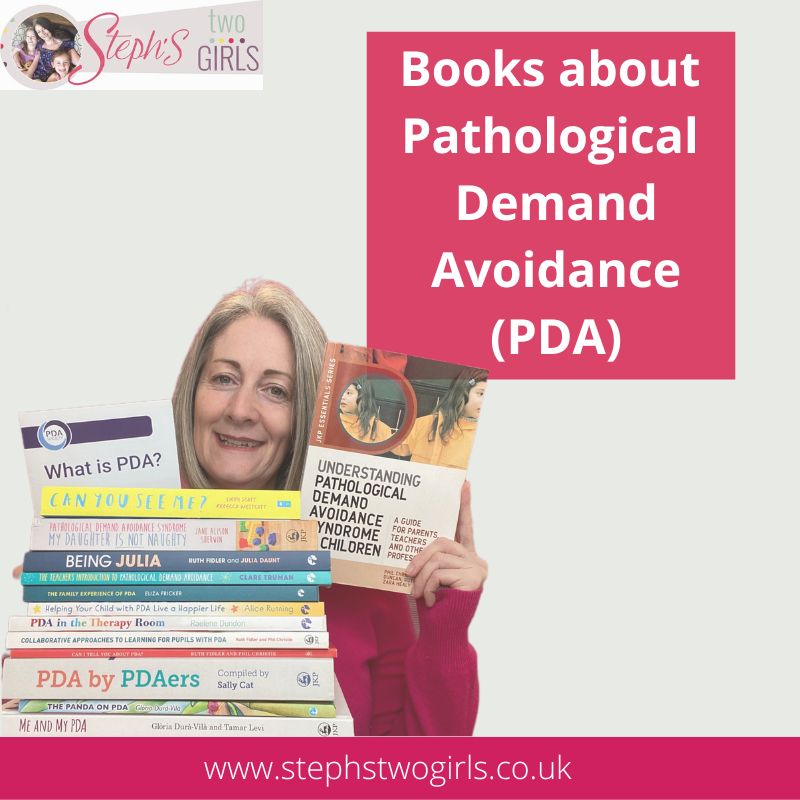
Alongside all the books on PDA that have already been published, there are also many good articles about PDA. I hope the following links can provide more interesting reading and research for those who are still not sure about the difference between demand avoidance and Pathological Demand Avoidance.
.....
The PDA Society is still top of my list when it comes to recommending information about Pathological Demand Avoidance. The PDA Society website has a comprehensive range of information and resources to help both families and professionals, and they also offer responses to more specific questions via their enquiry line.
.....
The first peer reviewed paper on PDA, written by Professor Newson. Published in the BMJ Journals, Archives of Disease in Childhood, in 2003:
.....
Phil Christie, author of Understanding Pathological Demand Avoidance Syndrome in Children (with Margaret Duncan, Ruth Fidler and Zara Healy) is a Consultant Child Psychologist who worked with Elizabeth Newson. I recommend reading this interview by adult PDAer Julia Daunt: An interview with Phil Christie
.....
The Neurodivergent Educator explores the topic of demand avoidance vs PDA more in But, aren’t we all a bit Demand Avoidant at times?
.....
Riko, adult PDAer who also blogs at Riko's blog:PDA and more, produced this great post about how PDA is different to ADA (Autistic Demand Avoidance): Autistic Demand Avoidance – an example
Here's a short extract from it:
Quite often, when you deal with the negativity around the thing the autistic person person is avoiding, they become able to manage it. For example if an autistic child is struggling to eat dinner because they cannot tolerate the sensation of tomatoes, removing the tomatoes and giving them food they can tolerate means they are now able to eat.
With PDA however, it’s usually not so much the task in question that is the problem as much as the fact that they need to do it. For example, they may love tomatoes and their dinner might be their favourite, but it’s the fact that they have to eat at all, or that they are expected to eat, or even that eating will make them feel good, that causes the demand avoidance.
ADA can seem rational, reasonable, and easier to fix where possible. Whereas PDA can seem unpredictable, unreasonable and difficult to fix as it often involves things we need and want to do with little way of altering it to make it easier.
.....
Tomlin Wilding - another adult PDAer who has also written great articles about PDA. Changing The name PDA is where the term Pervasive Drive for Autonomy is discussed.
.....
Kristy Forbes is an adult PDAer who writes and talks frequently and eloquently about PDA. In this post on her Facebook page, Kristy highlights the complexities and the need for distinction and more understanding: Pathological demand avoidance is not just...
.....
I love this interesting post by Dr. Neff, a late-in-life diagnosed Autistic-ADHD Psychologist: What's the Difference Between PDA and Demand Avoidance?
.....
I highly recommend all three of the informative papers published on the Help for Psychology website: Research & Journals.
Modification of the Coventry Grid Interview (Flackhill et al, 2017) to include the Pathological Demand Avoidant profile by Judy Eaton, Kathryn Duncan and Ellen Hesketh.
An exploration of the Pathological (or Extreme) Demand Avoidant profile in children referred for an autism diagnostic assessment using data from ADOS-2 assessments and their developmental histories byJudy Eaton and Kaylee Weaver.
Extreme/‘pathological’ demand avoidance: an overview written by Elizabeth O’Nions and Judy Eaton.
.....
*Quoted from Aggarwal A, Marwaha R. Oppositional Defiant Disorder. [Updated 2022 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557443/
**Quoted from Mohan L, Yilanli M, Ray S. Conduct Disorder. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470238/




















No comments:
Post a Comment
Comments are always very much appreciated and can really help the conversation go further...