There currently seems to be, and probably always will be, discussion over whether PDA is a good 'label' to give. For anyone who is not sure of the positives of having a specific diagnosis (a much better phrase than 'label'), I'd suggest a read through of all the previous weeks of this series as a starting point. I'm sure that all of these families do appreciate the understanding which comes with knowing more specifics about a diagnosis.
PDA is a type of autism, but the strategies which really work for this condition are different to those for classic autism, Aspergers or ODD.
This week's writer talks about a specific event of going to hospital with her daughter - something we had to experience ourselves a couple of years ago when we had a ten day stay in hospital with Sasha. The usual stresses of everyday life are of course magnified ten-fold in an environment such as this, and I could definitely relate to these words.
There is a building, likely very near to where you live, that may be considered to be ‘The House of Demands’. It’s not usually a very friendly looking building. It is large and complex. It contains many different people, however they do all share a goal - to help and heal those who are unwell or injured. It probably has a sign out the front that says ‘Hospital’.
Recently, my 9yr old daughter (who is diagnosed mild ASD and who I believe has PDA) and I had reason to spend some time in one of these buildings. It was the first time for her. Luckily, it was for a seemingly straightforward reason – to have routine dental work done. Due to my daughters’ anxiety and inability to cope with dental work being done in the chair at the dentist, we were having it done under a general anaesthetic at a hospital.
In my mind, the moments I thought would be the hardest for my girl (let’s call her Josie) would be connected with anxiety during the lead up. I was not even sure I would get her in the car to go to the hospital. Accordingly, we did lots of preparation before the day arrived. The hospital was great and allowed us a tour and meeting with some of the nurses, who also gave Josie an anaesthetic mask to take home and get familiar with. At this point I should explain that Josie is not on any regular medications at all, has an unusually low threshold for pain or discomfort (or even just the anticipation of them), and until you experience her in full meltdown you would barely even notice she is anything but 100% neurotypical.
The day arrived and aside from some mild anxiety about the fact that she wasn’t allowed to eat anything for breakfast (due to the upcoming anaesthetic) Josie was doing really well. We got out of the house and into the hospital with no problems at all. I was so proud of her. She had recently found a poster with the quote “She was unstoppable, not because she didn’t have fears or doubts, but because she continued despite them”. It has kind of become her mantra now and I am sure it helped her a lot that day.
As is usual for a hospital stay, when she was admitted the nurses came along and asked her lots of questions – ‘How are you?’, ‘What is your date of birth?’, ‘What are you here for?’ etc. All quite simple, but what I now recognise as the start of the intensive demands they inadvertently placed on her. Never mind the fact that she ‘had to’ have her teeth done in the first place, and it ‘had to’ happen at the hospital, and she ‘had to’ do as we were all asking, both directly and indirectly.
The first sign of her as yet hidden anxiety was when she had to put on the hospital gown. She hated it because it felt funny and she was worried people could see her underwear. After a minor meltdown with some swearing and hiding under the blankets (her, not me), and a discussion with a nurse, we decided a mild sedative would be helpful. The hospital gave me a liquid that I was able to convince her to drink. So, more demands: you need to drink this; you really do have to wear the gown etc. Josie and I came up with a plan where she would wear her T-shirt and a towel underneath the gown – this was OK with the hospital because neither of those contained any metal. Time to go to theatre and more questions from a multitude of nurses and doctors. I could sense it becoming a problem but the sedative helped and Josie went into theatre and managed the anaesthesia process with no problems. Phew. I was very shaky but a coffee and some quiet and I was OK. The worst was over, or so I thought.
It struck me at this point how many questions the staff at the hospital asked both me and Josie, and how demanding the whole process is for so many reasons. There is an expectation of how to behave, what to do, how to answer all the questions. These are all people she doesn’t know so she would be unsure of what answers they want; what is the right one. Add to this a total lack of control over the situation, sensory factors and a good dose of fear.
Back to the story….The next thing I knew a nurse came and got me to say Josie was out of theatre, it had all gone well and she had woken up in recovery. They also said she was a bit upset and confused and took me straight up to see her. Poor Josie was becoming very agitated. She had woken up in a strange place, with no familiar faces, lots of lights and machines, disoriented and likely feeling awful. A new nurse was talking to her trying to calm her down. I got in close and tried to calm her but unfortunately was unable to bring her back. Things escalated and she went into a full, violent meltdown. It culminated with the anaesthetist returning to sedate her.
When she woke up again a short time later I of course was right there, but so were a lot of other people. After a minute or two they started with the questions – ‘How are you feeling?’, ‘Do you want an ice block?’ - and the direct demands – ‘Lie still’, ‘Don’t touch the bandage on your arm’ etc. This continued for some time. Josie was upset and wanted to go back to our room immediately. Looking back I see that she was trying to gain some control and trying to help herself – she knows to get away from any situation where she feels anxiety building. The nurse told her she could as soon as she was more awake and settled (another demand). I told them I thought they would have some trouble getting the canula out of her arm so they decided to do that before we went back to the room. As soon as they told her what was happening her anxiety skyrocketed and she again went into full meltdown. More sedatives. Before she woke up again they removed the canula and anything else attached to her, then as she was stirring they took her back to our room. They closed the door behind us and left her and I to ourselves for at least an hour. It was perfect – no questions, no demands, no lights, no other people. She woke up fully and was much happier.
After a time she wanted something to eat. I said I would get a nurse but asked - was she ready for all the questions again? We made a joke and she asked me to pretend to be the nurse. We role played all the possible questions and demands. Then not one, but three, nurses came in to organise food. You can imagine how many questions they had!
In hindsight I should have thought more about how she might wake up from the anaesthetic. Although I had discussed her ASD with the hospital (PDA is virtually unheard of here, particularly in the rural area we live in), none of us had considered this part of the process. In the future I would be insisting that she wakes up in recovery with just me there, no other people, and that the curtains around her bed are drawn.
Although I realise that medical staff do need to ask patients certain questions to ascertain level of alertness and the like, I would love to see a scenario for patients such as Josie where the questions and demands are limited to those which are essential and/or presented in ways that hide the demanding aspect if at all possible. Hospitals really are ‘houses of demands’ and often for very good reason. I cannot praise the staff at our local hospital enough, they handled things very well considering the information they had. It was a huge learning experience for me, and future hospital visits will be taken with my eyes very much more open.
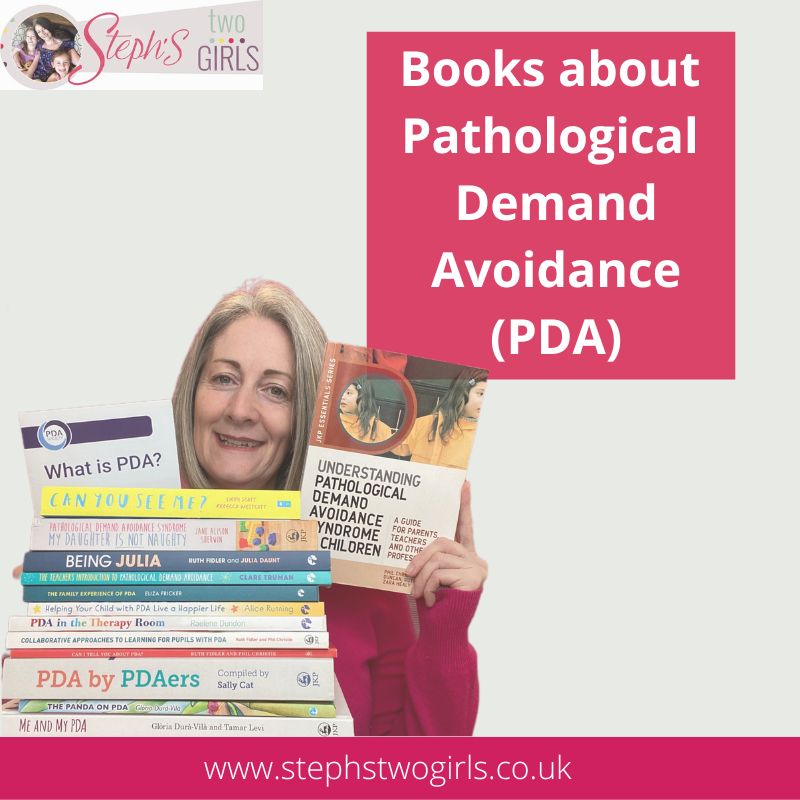
For more reading about what Pathological Demand Avoidance is, please see 'Challenging Behaviour and PDA', and for an idea of how to help please read Strategies For PDA.
PDA can often be mistaken for ODD (Oppositional Defiance Disorder) but there's a definite difference; more here: the difference between PDA and ODD.
If you feel up to sharing your own experiences with my readers to help spread understanding (this can be anonymously), please email stephstwogirls@gmail.com.
The PDA Society webpage has a huge range of information about Pathological Demand Avoidance, and there are also links to info on the PDA Resource website.
The PDA Society are holding a PDA conference in Birmingham on 18th April 2018 which I will be helping with - hope to see some of you there!
To find out more about our experiences, please check out our 'About Us' page. If you are looking or more information on Pathological Demand Avoidance, why not try some of these, my most popular posts?
What is PDA (Pathological Demand Avoidance)?
Ten things you need to know about Pathological Demand Avoidance
Does my child have Pathological Demand Avoidance?
The difference between PDA and ODD
Strategies for PDA (Pathological Demand Avoidance)
Pathological Demand Avoidance: Strategies for Schools
Challenging Behaviour and PDA
Is Pathological Demand Avoidance real?
To follow me on other social media channels, you can find me at the following links or click the icons below!




















No comments:
Post a Comment
Comments are always very much appreciated and can really help the conversation go further...